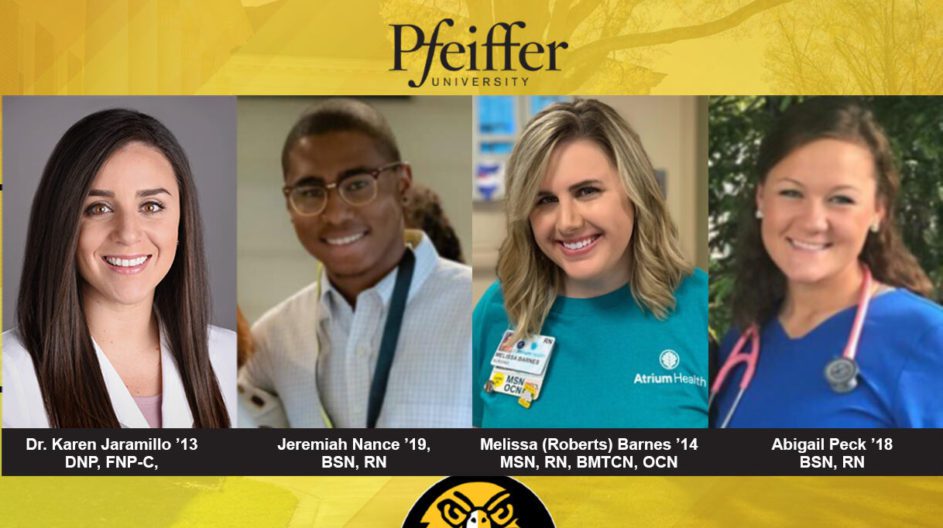
Pfeiffer Alumni on the Frontline of COVID-19
Before Abigail Peck ’18 BSN, RN begins a shift as an oncology nurse on the Hematology-Oncology floor of Duke University Hospital, she has read through three or four emails detailing how her employer is trying to stop the spread of the Coronavirus. She is also asked questions: Have you traveled outside the country? Do you have a fever? Have you been around someone who has a fever?
“You take it as a duty to others to answer those questions honestly,” said Peck, who earned a Bachelor of Science in nursing from Pfeiffer University. “If you have visible symptoms, you will not be allowed to get into the hospital.”
Once Peck begins work, she is reminded of extra-strict protocols governing the treatment of immunocompromised patients in her care. For example, they may not leave her unit for a procedure until they test negative for the virus.
There’s also a no-visitor rule in effect on Peck’s floor – which is especially difficult for her patients.
“No one wants to do chemo treatments for weeks without their family next to them,” she said. “We nurses have had to step it up with walking with our patients and caring even more so for their wellbeing in the absence of visitors.”
These days, the COVID-19 pandemic poses an array of unusual, daunting challenges, particularly for healthcare providers. Peck feels up to these challenges, crediting her training and support at Pfeiffer as a major reason. She said that the simulations of pandemic cases in a class on community health, taught by Dr. Dana Martin, familiarized her and her classmates with everything from controlling crowds of people to dealing with the confusions and frustrations that arise among patients and their family members.
“I’m grateful to have had a glimpse of that teaching at Pfeiffer,” she said. “My professors have also checked in on me throughout this time and it really goes to show how absolutely incredible my time at Pfeiffer was.”
Like Peck, Melissa (Roberts) Barnes ’14 MSN, RN, BMTCN, OCN is also dealing well with the COVID-19 pandemic because of her education at Pfeiffer. She manages a 43-member team as a nurse manager for Atrium Health in the inpatient hematology/blood and marrow transplant unit of the Carolinas Medical Center in Charlotte. Her immunocompromised patients await stem-cell transplants, having been diagnosed with such cancers as leukemia and lymphoma. Their risk of catching the Coronavirus is particularly high. So, they are no longer permitted to receive visitors.
Yes, many of Barnes’ patients are able to Skype, etc. with family and friends via smartphones. But, “it’s just not the same,” she said. “We sit with them a lot.”
In these situations, a course on therapeutic communication that Barnes took at Pfeiffer has proven to be particularly helpful. It taught her to “actively listen to our patients to hear what their needs are,” she said. It underscored the importance of a central tenant of Pfeiffer’s servant leadership ethos as it relates to nursing, namely that “we are taking care of the whole patient.”
Good therapeutic communication can take many forms. In instances where a nurse is sharing important information, it means employing a “teach-back method,” where a nurse would ask a patient to summarize what they just heard him or her say. It also recognizes that since not everyone absorbs information the same way, a nurse must discern the learning style that works best for a particular patient, such as watching a video or reading information.
As Barnes adapts to working during the very stressful COVID-19 pandemic, she keeps in mind the “de-stress techniques” that all her Pfeiffer professors taught her to practice: deep breathing, meditation, yoga, and exercising. She encourages a healthy work-life balance among those she manages, urging them to get outside for some fresh air, walk their dogs and play with their children.
Jeremiah Nance ’19, BSN, RN deals with stressful situations that have been made even more stressful because of COVID-19. That’s because he works in the Surgical Trauma Intensive Care Unit at Carolinas Medical Center Main in Charlotte. His patients are being treated for gunshot wounds and for injuries realized in car crashes and boating accidents. Before the pandemic, each one of these patients could be visited by three people; now, nobody is allowed to visit them.
“We’re going to treat them like human beings like we’d like to be treated,” Nance said.
He said that he deals with the Coronavirus threat at his hospital by being extra vigilant in following measures to limit its spread and by being a self-starter.
As a self-starter, Nance draws on the main principles at the heart of a course on research he took from Dr. Rachel Cozort: Look for all possible problems; then, examine all possible solutions that can help you adapt to the problems.
At least one Pfeiffer alumna is helping break new ground because of the COVID-19 pandemic. She’s Dr. Karen Jaramillo ’13 DNP, FNP-C, who serves as an Advanced Practice Provider for the Albemarle-based On-Site Clinic Stanly of Atrium Health Employer Solutions. She said her practice has moved to a “mostly telemedicine platform” to prevent the spread of infection among people sitting in a waiting room.
Telemedicine can take the form of a virtual video or an email consultation. “It didn’t become popular until the last couple of years; it’s booming because of COVID-19,” Jaramillo said. She added that’s “going to become the norm” for certain scenarios:
Telemedicine won’t replace onsite treatments for serious illnesses or injuries, but it will become the way to address such minor injuries as sprained ankles and small cuts and such sicknesses like the common cold, influenza and sinus infections. It can help determine the next steps; for example, can or should a clinic send someone to a patient’s home to take blood pressure or do blood work?
Thanks to telemedicine, women can more easily fill birth control prescriptions after they answer several questions and their medical records are thoroughly reviewed. Such a process can be very difficult to complete, if, as is often the case, a patient isn’t able to reach her primary care doctor.
Finally, as Jaramillo pointed out, Apple Watch apps are beginning to circulate more widely. They mean that patients can measure their heart rates without visiting a clinic or hospital.
One last note: Dr. Martha H. Bramlett RN, Ph.D. is an Associate Professor and Department Chair of the Department of Nursing at Pfeiffer. She stressed that Peck, Barnes, Nance and Jaramillo are just a few of the Pfeiffer nursing graduates “who are now on the frontline battling the COVID-19 pandemic with skill, courage, and grace.”
“The servant leadership of each of them is making a significant difference in very difficult times,” she said.
Ken Keuffel, who authored this article, has served as Pfeiffer’s Assistant Director of Communications since December 2019. He welcomes story ideas from Pfeiffer’s faculty, staff, students, alumni, and friends. The form for submitting story ideas is Story Idea/News Item Request Form.